Constant pain could be very uncomfortable for you and for the attachment to your baby during breastfeeding. It’s important to be able to identify the causes of the pain so you can treat them, go back to feeling well, and enjoy the process of bonding with your baby.
It is also important that you know that constant pain is not normal, the root cause of it can and should be identified so it can be treated.
We hope that after reading this you see that if you are experiencing constant pain while breastfeeding you are not alone and that you deserve to breastfeed without pain.
Nipple pain
Persistent nipple pain is one of the most common reasons why moms decide not to breastfeed anymore or at least not exclusively. It can also be the cause of psychological distress and interfere with activity, mood, sleep, and bonding with your baby.
Insufficient milk supply may be a secondary effect of nipple pain as a result of inhibition of the milk ejection reflex due to pain.
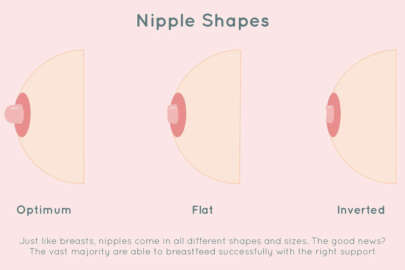
Nipple pain is attributed to positioning while breastfeeding and other causes like flat or inverted nipples, infant sucking action that causes nipple friction and infection. Nipple pain could be presented as:
- Nipple fissure: they are painful cracks in your nipple that can appear in one or both breasts, which are common, but not normal. Symptoms often appear during the second or third week after your baby is born. A cracked nipple is a sign that there’s too much pressure on your nipple tissue. Changes in your body during pregnancy and, especially, improper nursing techniques usually cause nipple fissures. You can treat fissures at home unless you experience complications like an infection or a fissure that won’t heal.
- Dry nipples: your nipples naturally make a lubricant to prevent drying, cracking, or infecting. To keep your nipples healthy it is important to avoid soaps and harsh washing, always dry them after shower and you can also rub a little breast milk on your nipple after feeding to protect it. Keep your nipples dry to prevent cracking and infection.
- Nipple lumps: is a mass that develops in your nipple, it is usually not serious; most go away without treatment, other may require a check from your doctor since engorged breasts, plugged milk ducts and mastitis can come with them, but nipple lumps aren’t the only symptom of them, so most of the time a breast lump is nothing to worry about.
- Nipple candida: is often described as burning and itching accompanied with pain; your nipples may appear bright pink and the areola may be reddened, dry or flaky. Signs may be present in your baby’s mouth or on your baby’s bottom or both. If you or your baby have candida you will both need to be treated.
- Nipple vasospasm: is what happens when the blood vessels supplying the nipple go into spasm and the blood that was flowing to the nipple gets reduced. Sometimes the nipple changes color to blue or purple and you may feel intense pain that worsens when you are cold.
- Nipple yeast infection
- Nipples peeling,
To prevent nipple pain an effective early lactation management is recommended, to get this done is important that the breastfeeding position is comfortable for you and for your baby and that it lets you have a good view of your nipple so you can make sure that there is a good latch (your baby’s mouth has your entire nipple as well as the surrounding areola). If you alternate positions it prevents your baby’s mouth it’s always putting pressure on the same spot.
Good hygiene it’s also important to prevent nipple pain: avoid using any harsh soap while washing to prevent a dry out, irritation or crack that can lead to pain.
* Correction of positioning and attachment is the most common experience-based recommendation for treatment of nipple pain especially within the first week of birth.
Should I maintain breastfeeding even when I’m experiencing nipple pain?
The answer is yes, you should continue to nurse on the affected breast. In the case that the location of the abscess (a painful pocket of pus) prevents direct breastfeeding, then it is recommended that you express milk from the affected breast while the incision is healing to prevent other complications.
Breast pain
Here we share the most common source of breast pain:
- Breast abscess: is a localized collection of pus within the breast. If you have one or feel like you may, you should reach your doctor so you can get an aspiration under local anesthetic or a more invasive incision depending on what your doctor finds convenient.
- Breast infection (mastitis): it can occur If the baby is not positioned correctly during breastfeeding, cracking (and soreness) can develop and it can lead to bacteria entering the milk ducts and causing an infection. An infected breast usually appears red and swollen and feels warm and tender. Doctors base the diagnosis on results of a physical examination.
- Hard boobs: it’s normal that when milk comes in, your breast gets full and firm which should pass if your baby is feeding well but in some cases breasts become hard like a rock and get a condition called breast engorgement.
Another thing that can be a cause of constant pain while breastfeeding is a milk or blood bleb/blister which is a blocked nipple pore that causes the milk to get stuck and become thick and hard which blocks milk flow.
To prevent breast pain while breastfeeding it’s important to avoid milk stasis (you can check out our article about mastitis to find more details about this). Pay attention to any signs of abscess, infection or hard boobs so you can consult your healthcare provider and get a proper treatment.
It is also important that you keep good hand hygiene when touching your breast and to maintain any equipment or fabric that touches your breast clean as well.
In Breastfeeding101 we hope that this gives you more clarity about some process and things that may concern you about constant pain while breastfeeding. We highly recommend that you reach your family doctor whenever you experience constant pain so you can get back on your feet and enjoy your breastfeeding journey with your baby.
If you want to deepen even more in this topic, you can consult some of the resources below that made this article possible:
Breast Abscess I National Library of Medicine
Breast Infection and Breast Abscess I MSD MANUAL
Breastfeeding – skin and nipple changes I MedlinePlus
Nipple fissure I Cleveland Clinic
Nipple candidiasis and painful lactation: an updated overview I Adv Dermatol Allergol
Nipple vasospasm I The royals women’s hospital
Kristen Howorko