When you are breastfeeding, you want to make sure that your baby is doing ok, but you also want to make sure that you are feeling good too.
Mastitis is a common and largely preventable condition that occurs in all populations and puts breastfeeding at risk.
But what exactly is Mastitis?
Mastitis is an inflammatory condition of the breast usually associated with breastfeeding that could be accompanied by infection but it doesn’t necessarily happen in every case. Is commonest in the second and third week postpartum, however it can occur at any stage of lactation.
Signs and symptoms of mastitis
- Breast may be swollen and feel warmth or tender to touch
- Breast lumps: a mass that develops in your breast
- Breast pain or burning sensation especially while breastfeeding
- Fever, chills; feeling ill, like when you get the flu
- Nipple discharge: refers to fluid leaking from the nipple area of one or both breasts
- Skin redness, often in a wedge-shaped pattern
What are the causes?
Basically, the two principal causes are milk stasis and infection.
- Milk stasis: is what happens when milk is not removed from the breast efficiently like when the breast is engorged soon after delivery or when the baby doesn’t remove all of the milk that is produced.
It could also happen when there is poor attachment of the breast, ineffective suckling, restriction of the frequency or duration of feeds and when blockage of milk ducts is present.
- Infection: if the breast is not completely empty after feedings a milk duct can become clogged; the blockage causes milk to back up, leading to breast infection. Studies have shown that without effective removal of milk, non-infectious mastitis was likely to progress to infectious mastitis.
Another way to get an infection could be through bacteria entering your breast from your skin’s surface or from your baby’s mouth, it can enter the milk ducts through a crack in the skin of your nipple or through a milk duct opening.
*Bacteria is often found in milk from asymptomatic breasts but its presence does not necessarily indicate infection.
Normal breast engorgement vs blocked
- An engorged breast is when the breast is overfilled with both milk and tissue fluid; the whole of both breasts is usually affected: they are enlarged, swollen and painful, the milk often does not flow easily, and it may be difficult for the baby to attach to suckle until swelling is reduced. The mom sometimes has a fever and feels ill.
- A blocked breast is when the breast has localized milk stasis; only a part of the breast is affected: it is shown by a painful lump in one breast, often with a patch of redness of the overlying skin, symptoms are rapidly relieved when the hard particulate material is expressed and milk is released from the affected part, the mom usually has no fever and feels well.
Infectious mastitis and non-infectious mastitis
Studies have shown that the signs and symptoms of infectious mastitis can´t be distinguished from non-infectious mastitis, so you should always check with your family doctor to make sure that you don’t have an infection if you are experiencing mastitis.
How to prevent Mastitis
The good news is that mastitis is largely preventable! Its prevention is based on good attachment and effective milk removal and to have this under control we want to share with you the follow recommendations:
- Your baby should be put to your breast immediately after delivery (so that milk stasis is avoided). But if this didn’t happen don’t worry, just pay attention if there is an early sign such as engorgement and blocked breast.
- Pay attention to any signs of milk stasis: always make sure you don’t have any lumps, pain or redness in your breast and if you notice any signs it is important that you rest. Also increase the frequency of breastfeeding and apply heat to the breast prior to feedings.
- Pay attention to other difficulties: if your baby is not eating or you feel that you have insufficient milk supply you should always ask your lactation consultant.
- Rest: fatigue is often a precursor to mastitis, so we encourage you to get a good rest and let your family know that breastfeeding moms may need more help so they can provide you with it.
- Good hygiene: always practice good hand hygiene, also breast pump equipment should be washed with soap and hot water after use.
Keep in mind that unrestricted and exclusive breastfeeding is an efficient way to prevent both milk stasis and spread of infection.
*Moms should contact their doctor if symptoms are not improving within 24 hours.
Treatment
A common question is: if I do have Mastitis should I stop breastfeeding? And the answer is no.
Some of the moms that are experiencing mastitis may stop breastfeeding because of the pain that they are experiencing or because they have been inappropriately advised by a health professional to do so but whenever possible breastfeeding should continue, both to improve milk removal and to help the condition to resolve, and for the benefit of your baby. We realized that if you are experiencing mastitis, breastfeeding could be painful, so we want to share with you the alternative of hand expressing and the way to do it.
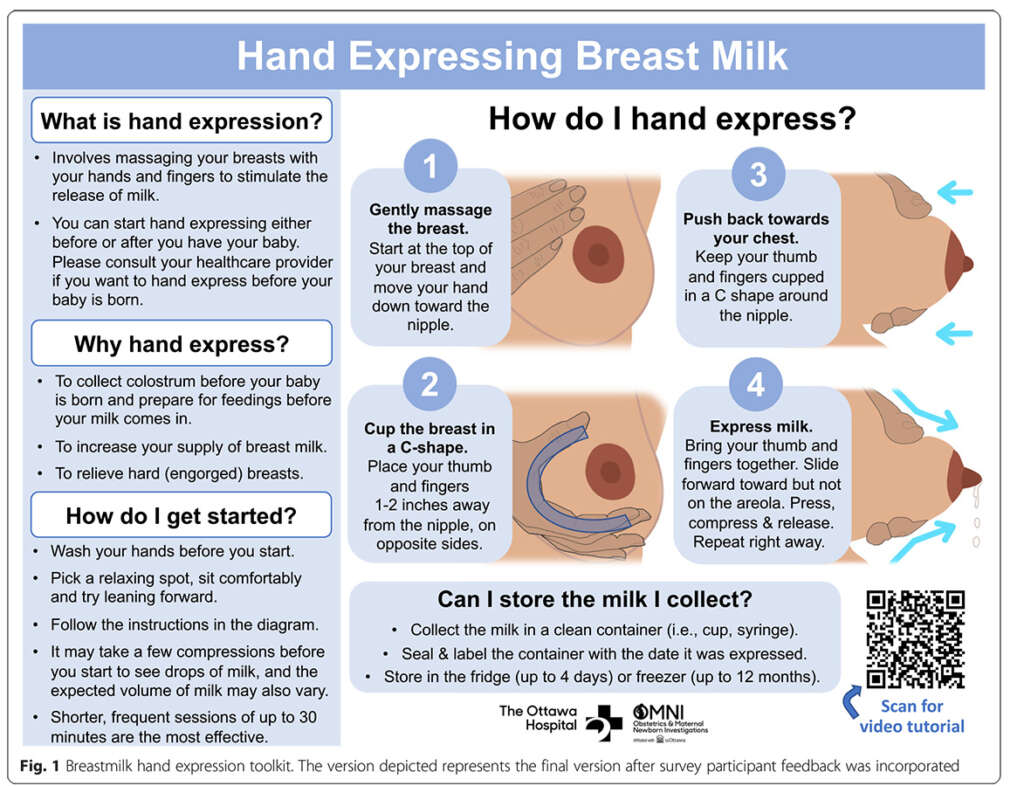
We also understand that if you have a clogged duct you are probably experiencing pain, for that we want to share with you the following video that brings you information about some things that you can do at home to treat it.
Regarding to bacteria, if present, bacterial or other infection should be treated with an appropriate antimicrobial agent, but this should be in addition to, and not an alternative to an effective milk removal such as the ones we have mentioned on this document. Continuing to breastfeed, even while taking medicine to treat mastitis, is better for you and your baby.
We hope this information has helped you to identify what mastitis is and what is not as well as the ways to prevent and treat it. We strongly recommend that you ask your specialist for any guide regarding your case, and we suggest you follow all of our content at Breastfeeding 101 to be informed on more topics involving breastfeeding.
If you want to deepen even more into the topic of mastitis, consult some of the resources that made this article possible:
ABM Clinical Protocol #4: Mastitis, Revised March 2014 I National library of Medicine
Acute Mastitis I National library of Medicine
Breast Infection: A Review of Diagnosis and Management Practices I National library of Medicine
Management of Mastitis in Breastfeeding Women I American Family Physician
Mastitis Causes and Management I WHO
Maternal Risk Factors for Lactation Mastitis: A Meta-analysis I Western Journal of Nursing Research
Kristen Howorko